-
Introduction To Knee Replacement Surgery
+ You need to have a clear idea about how your knee functions, and what might necessitate a knee replacement surgery - before actually opting to have the operation. Some basic concepts regarding knee replacement would be clarified over here:
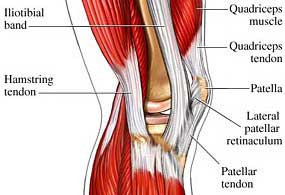
You need to have a clear idea about how your knee functions, and what might necessitate a knee replacement surgery - before actually opting to have the operation. Some basic concepts regarding knee replacement would be clarified over here:How does the knee joint work?
The knee joint comprises the femur (the lower portion of the thighbone). The joint operates by rotating on the patella (kneecap), and the upper section of the tibia (shinbone). The articular cartilage ensures that the bone movements remain smooth and properly cushioned. The patella slides on to the lower portion of the articular cartilage.
What is the synovial membrane?
The synovial membrane is the smooth and thin line of tissues, which protects all the adjoining areas near the knee. The membrane also releases a synovial fluid, which acts as a lubricating agent for the knee joint.
When the very first knee replacement surgery was performed?
The first knee replacement operation was successfully carried out in 1968. Since then, the techniques of knee replacement have become a lot more sophisticated. Knee replacement operation is currently regarded as one of the breakthroughs in medical science, in the 20th century.
What factors can necessitate a knee replacement surgery?
Acute arthritis (general osteoarthritis) more common among elderly people or arthritis caused by rheumatism and/or post-accident trauma).
- Unbearable knee pains (generally stemming from arthritis).
- Torn knee ligaments
- Tears in the meniscus
- Problems in knee cartilages
- Significant deformity
- Stiffness in the knee area
- External injuries
N.B: Contrary to what many believe, osteoporosis DOES NOT require a knee replacement surgery.
What are the general effects of a knee deformity?
- Acute pain, even while you are lying on the bed, or sitting on a chair
- Problems in locomotion, particularly while climbing stairs
- Relapse of knee pains, even after taking medications and following physiotherapy sessions
What are the types of knee replacement surgery?
Knee replacement surgery can be of two types, which are:
- Partial knee replacement surgery
- Total knee replacement surgery
What is the objective of a knee replacement surgery?
This operation is performed to insert medically approved plastic/metal joints, in place of your defective knee joints. When done in the proper manner, the surgery helps you to recover your powers of pain-free locomotion, within a relatively short time-span.
When is Total Knee Replacement necessary?
- When your knee pains are not getting reduced by general medications.
- When you require a quick and seamless relief from deep-seated arthritis problems.
- For removal of knee stiffness and deformities.
- When you are intolerant/allergic to antibiotics for reducing knee inflammation.
- When partial knee replacement would not properly rectify your condition (as decided upon by surgeons, physiotherapists, and other qualified medical experts).
WORD OF CAUTION:
Total knee replacement cannot make you fit enough to take part in athletic events, or other such highly strenuous activities. You need to stay away from certain activities, for the rest of your life. We will come to that later.
What does the knee replacement surgery involve?
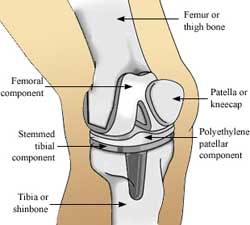
- Creating an incision along the middle portion of the affected leg(s)
- Analyzing the defective surfaces, to determine which parts of the knee joint have to be replaced
- Insertion of metal/plastic trough on the surface of the tibia
- Insertion of a stable metal shell, near the lower edge of the femur
- Protecting the kneecap with a plastic button (if required)
N.B: A standard knee replacement surgery requires a time of around two hours.
What are the types of knee prosthetics available?
- Prosthetics that are based on the natural ingrowths mechanism of bones
- Prosthetics that utilize medical cement to bind the joint components together
Note: Screws can be used with the first category of knee prosthetics, to keep the shinbone stabilized.
What are the basics of post-operative care after a knee replacement surgery?
- Continuous physical rehabilitation.
- Starting to walk with mobility supports (like canes, frames, and crutches).
- Gradual return to walking without external aids.
N.B: The total recovery process from a knee replacement operation takes a minimum of six weeks.
What are the activities you need to avoid after the surgery?
- High-impact sporting activities.
- Jogging and sprinting.
- Putting heavy pressure on the replaced joints in your knee.
You can, however, easily participate in light sporting activities, like bowling and playing golf. Have thorough knowledge about the knee replacement surgery, and the post-operative care required after the operation. Follow your doctor's advice – and ensure that the artificial joint(s) last for many years.
-
Types of Knee Replacements
+Many types of designs and materials are currently available. The knee joint is divided into three compartments for the purpose of description the medial [inner), the lateral [outer) and the kneecap compartments. Arthritis can affect one or more compartments of the knee joint. When two or all three compartments are damaged by arthritis, your surgeons will usually recommend a Total Knee Replacement.
There are two categories of Total Knee Replacement (TKR)
Fixed Bearing - the plastic cushion in this form of knee replacement is fixed to the metal tray on the tibial side of the knee joint.
Mobile Bearing - the plastic cushion is not firmly attached but is allowed to rotate on the tibial tray. This is a newer type of design. The wear rate of the plastic component is probably lower compared with fixed bearing design. However not all patients are suitable for a mobile bearing TKR.
Unicompartment - If only one compartment is affected by arthritis, your surgeon may recommend a Partial Knee replacement (Unicompartment knee Replacement). In this form of knee replacement, smaller components for the femur and tibia are used and the operation can be performed through a much smaller incision (Minimal Invasive Technique). Because of the less invasive nature of the operation, the recovery period after the surgery is much shorter and blood loss is significantly lower compared with a total knee replacement operation. Most patients are able to return home one or two days after the surgery.
Another advantage of unicompartment knee replacement is that the range of the motion tends to be better than that after a total knee replacement. Unicompartment knee replacements are however less durable than total knee replacements.
-
First Consultancy
+When you come for the first consultation for knee pain to Dr. Rakesh Rajput, it is advisable to come with a prior appointment unless it's an emergency, so that when you come to the clinic your time is spent fruitfully.
Kindly expect to spend about one hour and 30 minutes for your first consultation. This time is spent in obtaining detailed history, performing thorough clinical examination and for taking x-rays.
From the information obtained from history, clinical examination and x-rays, a knee score chart will be prepared for Dr. Rakesh Rajput's evaluation. After going through this score chart, Dr. Rakesh Rajput will discuss treatment modalities suitable for your knee problem.
Please remember:
- To mention if you have allergies of any sort, either to medicines or any other substances
- To bring the names of medicines that you take for diabetes, high blood pressure, asthma and medicines for pain relief and arthritis
- To bring previous x-rays, blood reports, examination findings of any other specialist doctor, if any
- To bring a note from your family physician giving a detailed description of your condition and medical history
-
X-Rays
+ Good quality x-rays in different positions are invaluable in arriving at correct diagnosis and for further management. Therefore, it is advisable to take x-rays under supervision of our staff for standardization.
Good quality x-rays in different positions are invaluable in arriving at correct diagnosis and for further management. Therefore, it is advisable to take x-rays under supervision of our staff for standardization.While you are waiting for the result of your X-ray, you may wish to view the computer program / video film pertaining to knee replacement surgery or you may go through this booklet.
Treatment for knee disorders is advised taking into consideration your age, medical history, the intensity of pain, findings of clinical examination and x-rays.
-
Conditons Requiring A Knee Replacement
+There are a number of conditions, which can result in a patient having to undergo hip replacement surgery. Perhaps the most common condition is osteoarthritis that is commonly referred to as 'wear and tear arthritis'. Osteoarthritis can occur with no previous history of injury to the hip joint. The hip simply 'wears out'. There may be a genetic tendency in some people that increases their chances of developing osteoarthritis.
 Avascular necrosis is another condition that could lead to hip replacement surgery. In this condition, the femoral head (ball) loses a portion of its blood supply and actually dies. This leads to collapse of the femoral head and degeneration of the hip joint. Avascular necrosis has been linked to alcoholism, fractures and dislocations of the hip and long-term cortisone treatment for other diseases.
Avascular necrosis is another condition that could lead to hip replacement surgery. In this condition, the femoral head (ball) loses a portion of its blood supply and actually dies. This leads to collapse of the femoral head and degeneration of the hip joint. Avascular necrosis has been linked to alcoholism, fractures and dislocations of the hip and long-term cortisone treatment for other diseases.Abnormalities of hip joint function, resulting from trauma to the hip, fracture of the hip, and some types of hip conditions that appear in childhood, such as congenital dysplasia of the hip (CDH) can lead to degeneration many years later. The mechanical abnormality leads to excessive wear and tear.
-
Preparation for Surgery
+You are asked to provide your surgeon with information regarding:
- Your general health
- Medications that you are taking
- Allergies.
- Previous operations.
- Bleeding disorders.
- Other bone and joint problems.
If you have any infections, your surgery may need to be postponed.
Medications:
You should cease taking any anti-inflammatory (arthritis) medicine, three weeks before coming to hospital.
You may need pain killer to help with pain relief during this time.
Diet:
Diet is especially important in times of stress such as Surgery. Be sure to include as many iron rich foods in your diet as possible, example: red meats, liver, beans, nuts and dried fruits.
If you are overweight, reducing weight will generally help your exercise program, make you feel better and reduce extra stress on your knee. Avoid crash dieting however as this is not healthy prior to surgery.
Blood transfusion:
Total joint replacement is major surgery, so you may require blood transfusion. Up to three units of blood may be needed.
Patients wishing to pre-donate autologous blood, should discuss this with their surgeon, and then arrange an appointment with Fortis Blood Bank.
-
Types of Implants
+Each section has an ODEP rating listed. This is an rating issued by a group of medical professionals. The number refers to the minimum number of years that the implant has been around ( 3 being a low number of years and 10 being the highest) and the letter refers to the quality of published data that supports the implant (a. being the best c. being the worst).
Types of Knee Replacement 

Uni-Condular Total knee 

Patello Femoral Revision Knee Partial Knee Replacement (Uni Condular)
 This type of treatment involves replacing just one side of the knee joint. Both the upper and lower parts of the knee are replaced, but unlike total knee replacement, just the worn out side is replaced. A metal implant is fixed (with or without bone cement) onto one of the upper side and on one side of the lower side of the knee; both of these articulate with a plastic material (polyethylene).
This type of treatment involves replacing just one side of the knee joint. Both the upper and lower parts of the knee are replaced, but unlike total knee replacement, just the worn out side is replaced. A metal implant is fixed (with or without bone cement) onto one of the upper side and on one side of the lower side of the knee; both of these articulate with a plastic material (polyethylene).This is a popular type of replacement and has had good clinical results over the past 15 years with around 4,000 being implanted in the UK every year, these replacements usually last around 10 years.
Total Knee Replacement
 Surgeons have performed total knee replacement surgery for over 40 years. Generally it is a very successful operation with over 80,000 being done every year, most total knee replacements last around 10-15 years. This surgery involves both sides of the knee joint being replaced, Both areas of bone are replaced with a metal implant and can be cemented or uncemented. These metal surfaces articulate with a piece of plastic (polyethylene) which can be fixed to the lower metal implant (tibial tray) or move on the surface of the tibial tray, the latter are known as mobile bearing knee replacements. In terms of how well they do in patients – they both perform very well. In knee replacement surgery, it is important to protect the plastic from wearing out as much as possible, as this is the weak area of the replacement. If the plastic wears out then it is likely that it will need to be replaced in the future.
Surgeons have performed total knee replacement surgery for over 40 years. Generally it is a very successful operation with over 80,000 being done every year, most total knee replacements last around 10-15 years. This surgery involves both sides of the knee joint being replaced, Both areas of bone are replaced with a metal implant and can be cemented or uncemented. These metal surfaces articulate with a piece of plastic (polyethylene) which can be fixed to the lower metal implant (tibial tray) or move on the surface of the tibial tray, the latter are known as mobile bearing knee replacements. In terms of how well they do in patients – they both perform very well. In knee replacement surgery, it is important to protect the plastic from wearing out as much as possible, as this is the weak area of the replacement. If the plastic wears out then it is likely that it will need to be replaced in the future.Partial Knee Replacement (Patello Femoral)
 This operation involves replacing some of the kneecap and the area which the knee cap moves. The area in which the kneecap (patella) moves is known as the patella groove, it is this area where a normal knee has a layer of cartilage. If this cartilage has worn out it can be painful and can be replaced with a metal surface.
This operation involves replacing some of the kneecap and the area which the knee cap moves. The area in which the kneecap (patella) moves is known as the patella groove, it is this area where a normal knee has a layer of cartilage. If this cartilage has worn out it can be painful and can be replaced with a metal surface.A plastic (polyethylene) disc is put on the back of the kneecap and articulates with the new metal surface. This type of operation has been conducted for over 15 years but in small numbers.
Re-do Knee (Revision Knee)
 If you have had previous knee surgery, which needs to be replaced, this is called revision surgery. A revision knee replacement is much the same as a total knee replacement. The surgeon has to remove the old implant and replace it with a new one. Once the old prosthesis is removed, there is often less bone available for fixation of the new replacement. Therefore, additional metalwork is often added to ensure a good fixation of the new implant. This extra metalwork comes in the form of metal augments, wedges, and stems. The augments and wedges are usually fixed to the new implant around the upper and lower sides of the knee to make up for any bone loss. The stems are attached to the implants themselves, if necessary, and fixed within the shaft of the thighbone or shinbone, to ensure good fixation and stability of the prosthesis.
If you have had previous knee surgery, which needs to be replaced, this is called revision surgery. A revision knee replacement is much the same as a total knee replacement. The surgeon has to remove the old implant and replace it with a new one. Once the old prosthesis is removed, there is often less bone available for fixation of the new replacement. Therefore, additional metalwork is often added to ensure a good fixation of the new implant. This extra metalwork comes in the form of metal augments, wedges, and stems. The augments and wedges are usually fixed to the new implant around the upper and lower sides of the knee to make up for any bone loss. The stems are attached to the implants themselves, if necessary, and fixed within the shaft of the thighbone or shinbone, to ensure good fixation and stability of the prosthesis. -
Investigations
+If you are advised knee replacement surgery you may require to undergo:
- Evaluation of status of your teeth, ear, nose, throat and kidneys to rule out hidden infection
- X-ray of your chest.
- ECG, 2D echo
Investigations as follows:

- CBC, ESR, Blood sugar fasting and after lunch.
- Blood group and Rh factor
- Kidney function tests, Liver function tests.
- Test for HIV.
- Test for Australia Antigen.
- Test to rule out Hepatitis C.
- Routine examination of your stool and urine.
- Special tests if indicated.
After assessing your reports, you will be referred to a physician for medical fitness, and to the anesthetist for evaluation.
Prior to surgery, you will be familiarized with the exercises, which you will be required to do after the surgery.
-
Operations
+If the surgery is scheduled for the morning, be ready after brushing your teeth. You will taken to the operation theatre at the time which will be informed the previous night.
If your surgery is scheduled for afternoon, you may be allowed tea/coffee and light breakfast early morning of the operation day.
While being taken to the operation theatre, please remember:
- To remove your denture
- To remove contact lenses.
- To remove spectacles.
- Not to carry cash or valuables.
Some medicines may be required to be taken by mouth on the morning of surgery with few sips of water and some injections may be administered prior to you being taken to the operation theatre.
 At the appointed time, you will be taken to the operation theatre. Here the anesthetist would put you to various monitors and check-up your heart, oxygen saturation and blood pressure. Before starting the anesthesia, an intravenous line in the forearm will be taken to administer various medications. As discussed previously you will be administered the anesthesia most suitable for you. If it is going to be epidural anesthesia, you will be made to sit and your lower back will the cleansed with an antiseptic solution. Then after numbing your skin, a thin tube will be inserted in your back with the help of a special needle.
At the appointed time, you will be taken to the operation theatre. Here the anesthetist would put you to various monitors and check-up your heart, oxygen saturation and blood pressure. Before starting the anesthesia, an intravenous line in the forearm will be taken to administer various medications. As discussed previously you will be administered the anesthesia most suitable for you. If it is going to be epidural anesthesia, you will be made to sit and your lower back will the cleansed with an antiseptic solution. Then after numbing your skin, a thin tube will be inserted in your back with the help of a special needle.Once you are anesthetised, a catheter may be put to ease passing urine. The actual preparation for the operation will start which will include thorough cleansing of the leg and applying the tourniquet at the root of your leg. Your leg will be cleaned once more with antiseptic solution and it will be covered with sterile drapes.
The actual surgery consists of entering the knee joint through an incision in front of the knee. The irregular cartilage of at the ends the thighbone, leg bone and the kneecap will be shaved by a power saw to the extent of 8-10 mm and the artificial parts will be fitted on the shaved bones with the help of substance called bone cement. During the surgery, the tension in the knee ligament will be adjusted so that the deformity present before the surgery will disappear completely. At the end of the surgery, the knee will be thoroughly washed with antiseptic solution and a thin plastic tube will be inserted in the joint to drain out the blood, which is likely to ooze during first 48 hours. After meticulously stitching up of the wound, a bulky compression dressing will be applied.
After some period of observation in the theatre complex, you will be shifted back to your room.
 If the surgery is carried out under epidural anesthesia, you will be allowed to take oral fluids within 2-4 hours after being brought to the room. On the day of surgery, you will continue to receive IV fluids.
If the surgery is carried out under epidural anesthesia, you will be allowed to take oral fluids within 2-4 hours after being brought to the room. On the day of surgery, you will continue to receive IV fluids.For pain relief, the epidural tube will be connected to a computerised infusion pump, through which you will receive continuous dose of pain relieving medications. From time-to-time you will administered injections and oral medications as per the doctors' instructions. If you have difficulty of any kind, please do not hesitate to call a nurse or a doctor. They will be always available to help you.
Some of the patients may require administration of oxygen for first 24 hours, while some patients may require monitoring in intensive care unit.
-
Post Operative Treatment
+Your Hospital Stay :
For a knee replacement procedure, it is of essence that you get admitted at a well-facilitated hospital, at least a couple of days before the operation. This will give you ample time to get used to the surroundings over there. All the necessary pre-operative medical tests can also be conducted with ease. We would here take a look at what would be your daily schedule on the day of the surgery, and the days preceding and succeeding it:
Day Before The Surgery:
- Heart and chest inspection by the doctor and the anesthetist.
- Preparation of the knee area for the surgical procedure (done by nurses/ward attendants)
- Discussion about the anesthetic to be used.
- Marking the precise area where the surgery needs to be done.
- Application of ‘pre-med' medications.
- Clarification of queries and doubts (if any) from your side.

Night Before The Surgery/Day Of Surgery:
The knee replacement surgery can be scheduled either during the morning, or during the afternoon. Depending on that, pre-operative food and drinks are recommended:
- If your surgery is in the morning, you will be put on a fast from midnight.
- If your surgery is in the afternoon, you will be probably given a light breakfast, and hygienic fluids – at around 7am.
N.B. à If you have to fast, you will find all details regarding the time of fasting from the Bookings Office of the hospital.
In addition, the following would be done on the night before/morning of the knee replacement surgery:
- Shaving the area around your hip. This might be necessary to minimize the chances of infections.
- A thorough shower on the night/morning (as applicable) before the surgery. The operation site needs to be absolutely clean.
- n Education Class, where you will be provided a packet of medically approved anti-bacterial liquid soap. Use it for your shower.
- Escorting you to the operation theater.
- Application of the anesthetic (as decided upon on the previous day).
N.B: A standard knee replacement surgery requires one to two hours of time.
Post-operative care:
- Injecting inside the walls of your abdomen. This is necessary to avoid internal blood clotting.
- Relocation to the Recovery Room.
- Providing medically recommended elastic stockings (TEDS) to you (done by nurses).
- Initiation of 1-2 drips in your arm, to ensure that the fluid balance in your body remains intact.
- Application of pain-relieving medications (in cases of significant post-operative pains).
- Monitoring your pulse rate, blood pressure level, and breathing pattern. Once all body metrics are stable, you will be shifted back to your ward.
- Consumption of ample fluids, in the days following the surgery.
- Removal of the drips.
- Monitoring the post-operative scar (which should reduce to a narrow, faded white line).
- Start of physiotherapy sessions.
- Walking with the help of supports (crutches or sticks). This process would continue for four to six weeks – until you get your strength back in the legs.
- Application of pain-alleviating medications (if required).
- Continuation of the Clexane injection (if required).
- Constant collaboration between your surgeon and your physiotherapist.
- Starting to walk without support.
- Discharge from the hospital.
For a knee replacement surgery, you need to stay at the hospital for 4-7 days. Once the post-operative treatment is complete, you will be able to resume your regular activities, as was your routine earlier.
-
After Surgery
+Immediately after your surgery
When you return to the ward from the recovery room you will have an IV drip in your arm for volume replacement, antibiotic therapy, and (if necessary) blood transfusion. After the operation the nursing staff will continue to measure your temperature, pulse and blood pressure. You will also have a small drain inserted into your knee. Special air filled calf compressors may be used after your operation to help your circulation by automatically inflating and deflating. It you feel up to it you may have something light to eat. You will feel very sleepy after your operation so our staff will assist you with your needs.
Your surgeon or the resident doctor will visit you regularly to discuss your surgery and progress. The physiotherapist wilt visits you on the first day and each day thereafter to help you with your walking and exercise program. Blood samples will be taken to check your condition after surgery and you will be able to resume your normal medications. You will also be give regular pain relief medication to maintain your level of comfort. During the first two days, you are Likely to be prescribed narcotic pain medications, as they are most effective in controlling pain. Some patients experience drowsiness, nausea and vomiting when given narcotic medication less regularly.
We will organize a normal diet for you as soon as you feel ready. The nurse will check the dressing on your wound daily and remove the small drain from your wound upon the doctor's instructions.
Wound care
Your wound must stay clean and dry before your sutures are removed. This means you will need to cover your knee when having showers, for example plastic bags or covers.
Showering & dressing
Initially the nurse will assist you to shower in a seated position using a commode chair. The nurse will demonstrate how to put your clothing more easily, i.e. dressing the affected leg first. You will need help with your TED stockings, socks and laces, for a while.
Duplex Doppler
During the course of your stay in hospital, a surveillance examination known as a Duplex Doppler may be conducted to diagnose any clots in the veins. This examination enables your doctors to treat deep vein thrombosis.
-
Exercise Program After Surgery
+The physiotherapist at the Education Class, to enable you to commence the exercise before your surgery, will demonstrate a home exercise program. This will help strengthen the muscles and keep joints mobile, reduce the risk of blood clots, prevent chest infection and subsequently assist to speed your recovery.
Breathing exercises
Regular deep breathing and coughing practiced in the seated position will help keep your lungs clear and free from congestion and reduce the risk of infection. Take ten deep breaths, holding each breath for 3 seconds, followed by a strong cough each hour. Smokers should stop smoking two weeks prior to their surgery, so the lungs will be cleared of phlegm, as to reduce the risk of chest complications following surgery.
Activity program after surgery
Exercise is a critical component of your recovery, particularly during the first few weeks after surgery. You should be able to resume most normal light activities of daily living within three to six weeks after surgery. Some discomfort with activity, and at night, is common for several weeks.
Your activity program, which begins during your hospital stay, should include:
- A graduated walking program initially in your home and later outside.
- Walking program to stowing increases your mobility and endurance
- Resuming other normal household activities
- Resuming sitting, standing, walking up and down stairs
- Specific exercise several times a day to restore movement
- Specific exercise several times a day to strengthen your hip joint
- Outpatient physiotherapy
Stairs
When walking up the stairs, you always put your non-operated leg up first, then followed by your operated leg and walking aid together.
When walking down the stairs, you need to put the operated leg and walking aid down first, and then followed by your non-operated leg.
How is your new knee different
You may feel numbness in the skin around the incision. You also may feel some stiffness, particularly with excessive bending. These differences often diminish with time and most patients find these are minor compared to the pain and limited function they experienced before surgery.
Your new knees may activate metal detectors required for security in airports and some buildings. Tell the security agent about your knee replacement if the alarm is activated. You may also ask your orthopedic surgeon for a card confirming that you have an artificial knee.
After surgery, make sure you also do the following:
- Participate in a regular tight exercise program to maintain proper strength and mobility of your new knee.
- Take special precautions to avoid fall and injuries
- Notify your dentist that you have had a knee replacement. You should be given antibiotics before all dental surgery for the rest of your life.
- Should you sustain cuts or abrasions on the leg ensure that they receive proper medical attention. Infections from sores or wounds in the leg could cause an infection in the knee joint.
- Urine infections should also receive prompt medical attention
- See your orthopedic surgeon for routine follow-up examinations and x-rays.
Before leaving the hospital:
Your doctor will discharge you from hospital depending on your condition and mobility.
- Getting out of bed and a chair
- Going to the bathroom
- Attending to your own toilet and showering needs
- Walking with the assistance of an aid for about 50-60 meters
- Walking up and down stairs with assistance of an aid
- Knowing your knee precautions.
We will be giving you:
- A prescription for your discharge medications
- A follow up appointment to see your specialist
- A referral to physiotherapist
- Form for Doppler test if required.
-
After Discharge from Hospital
+Going home
You will need to continue to do your exercises after leaving hospital. Your surgeon, or Fortis hospital by phone on or go to the emergency department at Fortis Hospital:
- Chest pain
- Pain or swelling in the calf
- Wound becoming red or oozing
- Pain not relieved by medication
- Fever
Daily activities and managing at home
The physiotherapist will discuss with you how to manage daily activities a home after your operation. Here are a few hints to make sure you will be safe and independent at home.
Safety
- Make sure there is a clear passageway around your home
- Removal loose mats/rugs from the floor
- Make sure there are no electrical cords lying across the floor
- Use a firm chair with arms- makes sure it is not too low.
Transport
- Allow plenty of room and sit in the front seat.
- Ask your physiotherapist to show you the correct and easiest way of getting in and out of the car
- Ask your doctor first before driving
Sexual activity
- Let your partner take an active role
- You may find some positions more comfortable than others due to the discomfort of your wound
Rest
- Plan to have frequent rest breaks
Leisure
- Avoid kneeling to perform leisure activities
- Your physiotherapist will discuss your leisure activities with you and provide advice regarding safe resumption.
Showering
- A shower is preferable to a bath because it is easier to get in and out If you have a shower over the bath, you may need to use a bath board and a hand held shower
- This can be arranged if necessary
- Sit down to shower
- Always use a non -slip mat
- Don't use a tap or soap holder to hold onto as they may be slippery and are not strong enough
- Use soap on a rope or soap in a stocking to save picking dropped soap
Dressing
- Sit down to get dressed
- A long handled shoehorn will help you to put shoes on
- A sock gutter will help you to put socks on
- Avoid crossing your legs
- An easy reached or long handled BBO tongs will help you to pick up objects off the floor
Household tasks
- Avoid putting things on the floor, put them on a bench or table
- Use long handled aids such as BBQ Tongs
- Avoid bending and lifting, store items used daily on a bench or at waist height.
- Plan to do small tasks each day and not everything in one day
Washing
- Wash in small quantities
- Use a trolley instead of carrying the basket
- Keep pegs at working height
Ironing
- Use an ironing board
- Sit on a stool
Bed making
- Have your bed moved from the wall for easy access
- Use fitted sheets and continental quits if available
- Avoid extension and hip flexion when tucking in sheets and blankets. If you or your families have any concerns about managing at home after your operation, please discuss these with your nurse or physiotherapist
Driving
- You can resume driving following advice from your surgeon.
- Depending on your type of surgery this could be between 2- 4 weeks.
Home safety checklist
After surgery, you'll have special needs. You'll need to be careful getting around your home you'll need to prevent accidents. Read each item in this checklist carefully. Correct any items you think are problems in your home. Remember, only you can prevent accidents that prolong your recovery.
Walking
- Remove throw rugs whenever possible to avoid tripping
- If you can't remove throw rugs, use rugs with non skid backing to avoid slipping
- Make the transition between types of flooring as even and
- ecuring as possible to prevent tripping
Stairs
- The rise between steps should ideally be no more than 5 inches/15cm
- Make sure handrails are well -anchored on both sides of the stairway
- Non skid treads can be placed on wooden stairs to prevent slipping
- Make sure carpeting on stairs is secure
Furniture layout
- Arrange furniture so that pathway are not cluttered
- Chairs and tables need to be study and stable enough to support a person leaning on them
- Avoid furniture with sharp edges and corners. If furniture's does have sharp edges or corners, pad it.
- Chairs with arm rests and high backs provide more support when sitting and more leverage when getting in and out of a chair
- Bed/chairs should be 19-21 inches/47-53cm from the floor
Lighting
- Be sure that your lighting is ample to prevent falls and assure that you can Read medication [abet and instruction easily
- Light switches should be immediately accessible upon a room
- Good lighting for hallways, stairs and bathroom is especially important
Sliding glass doors
- Mark sliding glass doors with stickers to prevent someone from walking through them.
Bathroom safety
Toilet
- Use an elevated toilet seat or commode to ease getting on and off the toilet
- Install grab bars around the toilet if you need more support getting on and off of the toilet
Bath
- Install skid-resistant strips or a rubber mat
- Use a bath seat if it is difficult to stand during a shower or too difficult to get up out of the bath
- Install grab bars on the side of the bath or shower for balance
- Install hand-held shower
- Do not use the soap dish or towel bar for balance as these can easily pull out of the wall
- Remove sliding shower door
Doors
- Avoid locking bathroom doors or use only locks that can be opened from both sides when you
- May need assistance in the bathroom
-
Risks & Complications
+Total knee surgery is safe and effective. The vast majority of patients who undergo total knee replacement surgery do not experience complications. Your orthopaedic surgeon and the hospital staff will do their best to minimize the risk of these complications from occurring. Chronic illnesses may increase the potential for complications. Although uncommon, when these complications occur, they can or limit your full recovery.
The following write-up describes some of the complications associated with total knee replacement surgery. This list is not exhaustive and your surgeon and his clinical assistants would discuss with you other possible complications. Please ask your surgeon if you have any questions about this or other aspects of the surgery.
Anesthetic complications
Replacement surgery in India your anesthetist is the best person to discuss this with you prior to your surgery. If you have any questions regarding the type of anesthesia you are going to receive, or if you have had previous problems with anesthesia, please do not forget to let your anesthetist know. Some medications interact with anesthetic agents, so it is necessary to inform your anesthetist of any medication you are taking.
Infection
The risk of infection after total knee replacement is between 1-2%. Infection is more common amongst patients who have a condition affecting their immune system. Infections may be superficial or deep. Deep infections are more serious and further surgical treatment and prolonged hospitalization may be required for uncontrolled infections. This is fortunately very rare. Treatment of infection might mean multiple trips to operating theater for drainage and cleaning of wound. If the infection is deep, your surgeon might elect to remove all the metal and plastic parts, together with all non-visible tissues. Depending on the type and severity of infection, antibiotics may be administered through the veins for a period of two to six weeks. When the infection is controlled, a new prosthesis can then be implanted.
Deep venous thrombosis and pulmonary embolism
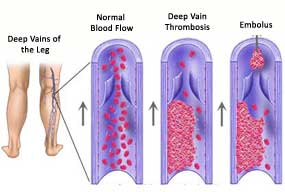 Knee replacement in India, clotting of the blood in the veins of the legs is a recognized complication and perhaps the most common complication of total knee replacement surgery. These clots, unfortunately, sometimes get detached and travel in the blood stream to reach the lungs. This is known as a pulmonary embolism. This is a serious condition and life is sometimes at risk. Every effort is made to try to minimize the occurrence of these complications. These measures include daily or twice daily injections of a substance into the abdominal wall that thins the blood and reduces the risk of clotting. Your medical condition and other considerations will influence the use and dosage of this substance (prophylactic anti - coagulants). You will be provided with white compressive leg stockings to wear. Usually these stockings are worn for a total period of six weeks.
Knee replacement in India, clotting of the blood in the veins of the legs is a recognized complication and perhaps the most common complication of total knee replacement surgery. These clots, unfortunately, sometimes get detached and travel in the blood stream to reach the lungs. This is known as a pulmonary embolism. This is a serious condition and life is sometimes at risk. Every effort is made to try to minimize the occurrence of these complications. These measures include daily or twice daily injections of a substance into the abdominal wall that thins the blood and reduces the risk of clotting. Your medical condition and other considerations will influence the use and dosage of this substance (prophylactic anti - coagulants). You will be provided with white compressive leg stockings to wear. Usually these stockings are worn for a total period of six weeks.Clots in the lungs cause shortness of breath and chest pain. Inform the nursing staff, if you experience such symptoms. Treatment is by oxygenation and administration of blood thinners
Instability/ Dislocation of the kneecap
Hip replacement surgery in India, dislocation of the kneecap, or more rarely dislocation of the plastic cushion (in a mobile bearing knee replacement), can happen after total knee replacement. In case the kneecap does shift to the outer portion of the knee, severe pains might ensue. Realignment of the kneecap generally requires a further surgical procedure. At times dislocation results from erroneous positioning of the components and a revision operation may be necessary. However, with rapid advancements in the techniques for knee replacements, such dislocation risks have reduced considerably.
Fat embolis
Fat from the bone marrow can reach circulation and could travel to the lungs. This condition is quite similar to the previous complication of pulmonary embolism. That is why it is called a fat embolism. The symptoms are quite similar to those of pulmonary embolism.
Mobility Loss
 Post-operative stiffness can lead to a certain degree of mobility loss for the patients. Instead of the general knee joint mobility of 0-135 degrees, a person who has undergone surgery can achieve mobility only up to 110 degrees. However, with the increasing popularity of medically approved ‘high-flex' knees and the implants they contain, such mobility losses can be reduced to a minimum. The amount of mobility loss also depends on how flexible the knee joint of a patient was, before the operation.
Post-operative stiffness can lead to a certain degree of mobility loss for the patients. Instead of the general knee joint mobility of 0-135 degrees, a person who has undergone surgery can achieve mobility only up to 110 degrees. However, with the increasing popularity of medically approved ‘high-flex' knees and the implants they contain, such mobility losses can be reduced to a minimum. The amount of mobility loss also depends on how flexible the knee joint of a patient was, before the operation.Wound complications
Wound necrosis (which means that the wound edges turn black) and wound breakdown (which means that the surgical wound opens up) are two complications that sometimes occur. When these complications occur, a further operation to repair the wound may be necessary.
General medical problems
General medical complications can sometimes occur after any major surgery. These complications includes heart attack, strokes, lung collapse, pneumonia, various heart problems, kidney dysfunction and bed sores.
Pressure sores
Pressure sores, especially of the heel area, can develop within 24 hours of lying in the bed. They can be prevented by avoiding inactivity in bed. It is necessary that you relieve pressure from the heel and buttocks (sacral area) regularly. If you notice sensations of burning or pain in pressure areas, you should inform your doctor or the nursing staff.
Vessel and nerve injury
A number of large blood vessels and the main nerves that supply the lower limb surround the knee. These structures are always at risk from stretching or direct injury. Every precaution is taken to minimize the risk of these structures. The lateral popliteal nerve is at particular risk of injury in total knee replacement surgery. Other nerves and vessels can be compromised during surgery. Nerve and vessel injuries can result in long-term disability.
It is very common for some superficial sensory nerves to be divided during surgical exposure of the knee. This can result in altered or reduced sensation over the front of the knee. Occasionally a swelling of the nerves develops. This uncommon complication may cause hypersensitivity of the skin or wound.
Fractures
Fractures of the shaft of the femur and the tibial bone occur sometimes, especially when the bones are soft and weak. The complication is more common during revision knee surgery. Fractures also occur if you sustain a heavy fall following surgery.
Loosening and wear
 Your new knee replacement is not expected to last forever. More than 95% of knee replacements are expected to be functioning well after fifteen years from implantation. You can help to prolong the life expectancy of your knee by looking after it. This means that you should remain active but not over active. Squatting, heavy impact sports and activities, and running should be avoided. Should the prosthesis loosen or wear excessively, a revision operation may be needed to treat the problem.
Your new knee replacement is not expected to last forever. More than 95% of knee replacements are expected to be functioning well after fifteen years from implantation. You can help to prolong the life expectancy of your knee by looking after it. This means that you should remain active but not over active. Squatting, heavy impact sports and activities, and running should be avoided. Should the prosthesis loosen or wear excessively, a revision operation may be needed to treat the problem.Knee alignment
In performing a total knee replacement, your surgeon aims to align the knee to take into account the weight - bearing axis of the leg. A difference in alignment of the knees is common after surgery particularly if only one knee is replaced.
Limp
Most patients have a mild limp after surgery and for about six months. The limp usually disappears or at least subsides significantly after six months.
Stiffness
Your knee is expected to move from being fully straight to at least ninety degrees of bending. There is an element of unpredictability about the range of motion after total knee replacement surgery. Some knees are stiffer than others are. If your surgeon is not happy with the amount of bending you are getting, he may decide to perform a manipulation of the knee under anesthetic and try to improve the range of motion in your knee. This is usually done between four and eight weeks after the operation.
-
FAQ
+If you are advised Knee Surface Replacement surgery, you may want to know more details about it. Here we list the most commonly asked questions about Knee Replacement (commonly called Total Knee Replacement) and their answers. If you want any further clarification, please do not hesitate to ask either Dr. Rakesh Rajput or one of his associates.

Q. At what age does arthritis pain start?
A. Above the age of 35, about 30% of people suffer from painful joints due to arthritis.
Q. What are the types of Arthritis?
A. There are mainly two types of arthritis. Osteoarthrosis means wear and tear due to ageing and joint abuse. The other common type of arthritis is called Rheumatoid arthritis, which behaves like an allergy.
Q. At what age can joint replacement be done? Can it be done for children?
A. Joint replacement is ideally done for patient above the age of 60 years.It may be done between ages of 40 and 60. It is rarely done between ages of 20 and 40. It is never done in children.
Q. What are the commonly used materials for joint replacement?
A. Commonly used materials for joint replacement are stainless called Cobalt Chrome Alloy and Plastic called Ultra High Molecular Weight High Density Polyethylene.
Q. What is the average time taken for joint replacement surgery?
A. The average time taken for joint replacement surgery is 1 hour 20 minutes
Q. What is the average hospital stay recommended after joint replacement?
A. The hospital stay is for five days after single joint replacement.
Q. When do exercise programme start after joint replacement?
A. Exercises on CPM start within a day after joint replacement, while walking is started 2 - 3 days after joint replacement.
Q. Does one need some support of walker or stick after joint replacement?
A. You may need support of walker or walking stick after joint replacement depending on whether other joints are affected.
Q. Can a person with diabetes, high blood pressure, heart trouble undergo joint replacement?
A. Even a person with diabetes, high blood pressure, heart trouble can safely undergo joint replacement surgery under medical supervision.
Q. What are the precautions to be used after joint replacement?
A. It is advisable to use commode, avoid sitting on floor, jogging, running and fast sports after joint replacement surgery. Moderate speed walking, climbing stairs and swimming are permitted.
Q. Can a patient be operated for both joint replacement at the same time?
A. Usually one joint is resurfaced at a time, but if the patient is fit, both knees or both hips may be resurfaced in one sitting.
Our centre has performed the largest number of successful two knee surgeries in one sitting.
Q. What are the common complications after joint replacement?
A. The complications after joint replacement are Deep vein thrombosis and Infection.
Q. What precautions are taken to prevent these complications?
A. To prevent deep vein thrombosis, early exercises are started. At our centre a special instrument called "Calf compression device" is applied to legs, which gently massages the legs and pushes the blood back towards the heart, thereby preventing blood clots.In some patients specialised medication is administered. At our centre to prevent infection,the surgical team wears special gowns called "Space suits". Also the surgery is carried out in specialised operation theatre and antibiotics are given pre-operatively.
Q. Can these operations be done in any Nursing home or Hospital?
A. No, This is a specialised surgery, which requires special set up including proper operation theatre, pre-operative intensive care unit, trained nurses and technicians and expert physiotherapist to achieve desired results.
Q. How much does the surgery cost?
A. The cost depends on the type of Implant, the type of room that you select and your medical condition. Before surgery, a budget can be drawn out.
Q. Is it covered under Mediclaim?
A. That will depend on the Mediclaim policy.

Dr. Rakesh Rajput
MBBS (Cal), MS Orth (Cal), FRCS (Glasgow)
MCh Orth (UK), FRCS Trauma & Orth (UK)
Director and HOD, Dept. of Orthopedics CMRI Hospital, Kolkata President AOPAS Specialist in Total Knee Replacement, Hip Replacement, Joint Replacement, Arthritis, Arthroscopy, Pelvic & Acetabular Trauma |









